Clinical Information
Cerebrovascular Disease
Diseases that are caused by some abnormality in the blood vessels of the brain are collectively called “cerebrovascular diseases”.
A sudden onset of stroke is called a stroke, which includes subarachnoid hemorrhage, cerebral hemorrhage and cerebral infarction.
In this section, we will introduce the diseases of cerebrovascular disorders and explain the current approach to treatment.
Direct surgery for cerebrovascular disorders is performed by a technical advisor of the Japanese Society of Stroke Surgery (Tomoya Kamide). In addition to conventional surgery, endovascular surgery is widely used. We have one neuroendovascular surgeon (Kouichi Misaki) and two specialists (Tomoya Kamide and Akifumi Yoshikawa) to perform endovascular operations. In addition, we also perform many advanced treatments (hybrid treatment) for highly difficult cases by performing both direct-direct surgery and endovascular surgery at the same time. We are also actively involved in the support of facilities in Ishikawa and the Hokuriku region by visiting them for treatment.
Cerebral aneurysm
Subarachnoid hemorrhage occurs in about 20-25 per 100,000 people each year, with 30-40% of these deaths occurring each year, and the majority of subarachnoid hemorrhages are caused by ruptured brain aneurysms.
If a ruptured cerebral aneurysm is identified, surgery is performed to prevent re-bleeding.
There are two main methods of surgery: one is an open head clipping procedure and the other is an end-aneurysm embolization (endovascular treatment).
Also, with the recent proliferation of brain scans, more aneurysms before they rupture, or so-called unruptured brain aneurysms, are being found than ever before.
Unruptured cerebral aneurysms must first be carefully evaluated for treatment, but basically, as with ruptured aneurysms, they can be treated with either open clipping or endovascular treatment.
① Clipping

Open craniotomy clipping was first performed in the 1930s and became widespread with the introduction of surgical microscopy in the 1970s, and is still performed as a standard of care. This surgery prevents rupture by directly examining the cerebral aneurysm and surrounding structures through open surgery, and then clipping the root (neck) of the aneurysm with a titanium clip to completely block blood flow to the aneurysm.
The greatest advantage of the clipping procedure is that recurrence of the clipped aneurysm is very unlikely.
② Endovascular Surgery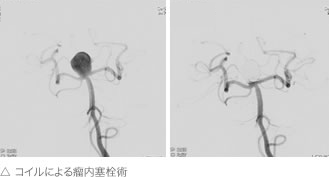
Endvascular embolization is a method of treating an aneurysm without having to perform a craniotomy. In what is called endovascular surgery, a microcatheter of less than 1 mm is advanced into the brain aneurysm and a platinum coil is placed inside the aneurysm through the catheter to prevent it from rupturing.
Most aneurysms can be treated with conventional clipping and endovascular surgery, but special treatment may be required for giant brain aneurysms, dissecting aneurysms and wide neck aneurysms. If the neck is wide, embolization may not allow the coils to fit well within the aneurysm and deviate toward the mother artery. If the deviation is severe, a thrombus may occur or the mother’s artery may become occluded, which may lead to serious complications. Such wide neck aneurysms are often safer if they can be treated with an open head clipping technique. However, if the patient is too old to be treated by craniotomy, endovascular surgery is still performed. In such cases, a balloon catheter may be used to hold the coil while embolization is performed, or a mesh tube may be placed in the neck to prevent the coil, called a stent, from deviating. In some cases of brain aneurysms, we have also introduced a state-of-the-art treatment using a special stent (flow diverter) called a pipeline.
The first endovascular treatment was performed in the early 1990s and was approved in Japan in 1997. Kanazawa University Neurosurgery has been performing endovascular surgery since 1997 and offers a high level of treatment based on its experience in over 600 cases of endovascular treatment of aneurysms. The main advantage of this treatment is that it is less invasive and therefore less physically demanding, but may need to be re-treated at a later date due to recurrence.
The two treatment methods, cerebral aneurysm clipping and endovascular surgery, do not mean that one is better than the other. If the characteristics of both treatments are understood and treated with the correct indications, the patient’s prognosis will be even better.
③ Aneurysm treatment with bypass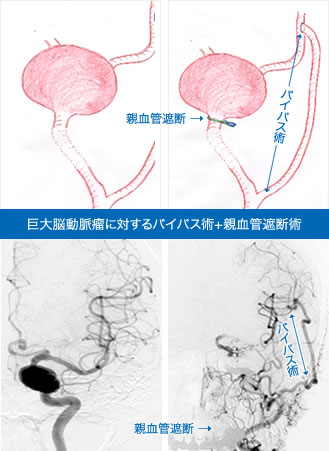
Some aneurysms are not amenable to normal clipping or intra-aneurysm embolization.
Specifically, these include giant brain aneurysms, bacterial aneurysms, and some dissecting aneurysms.
For those aneurysms, the entire mother artery must be occluded. Blocking the mother artery means that blood flow to its periphery will be lost.
For example, if the internal carotid artery must be occluded, blood flow to the ipsilateral middle cerebral artery and the anterior cerebral artery may be lost.
Normally there is collateral blood flow, which is blood flowing in from other sources, so it doesn’t necessarily result in a stroke, but if there is inadequate collateral blood flow, a bypass is necessary to compensate.
In such cases, we perform a preoperative balloon occlusion test to determine the need for bypass. We can perform either low-flow bypass (using the shallow temporal artery) or high-flow bypass (using the radial or great saphenous vein) depending on the blood flow required.
Ischemic Cerebrovascular Disease
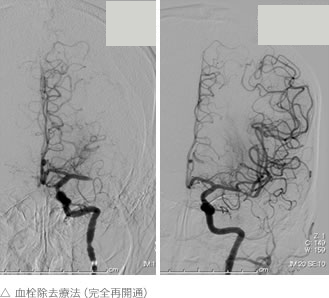
① Treatment of Acute Stroke
A stroke is a brain injury caused by a blood clot in a cerebral blood vessel.
In severe cases, the patient may be bedridden, in a vegetative state, or even die.
Patients whose large blood vessels in the brain (the main brain artery) are clogged are given intravenous injections of a clot-busting drug called alteplase (tPA) within 4 hours and 30 minutes of the onset of the disease.
However, if the clot does not dissolve even with this medication, or if it cannot be administered, endovascular treatment is performed.
A catheter is inserted through the femoral artery at the base of the foot and advanced to the occluded vessel, where the thrombus is retrieved (mechanical reopening therapy).
This treatment is time-consuming, but it has become possible to save lives and reduce the aftereffects if it is performed in the hyperacute phase.
When a patient with occlusion of the main brainstem artery is transported to each hospital, the Kanazawa University Neurosurgery Department receives the images, and if the patient is eligible for reopening of the acute phase of treatment, the images are transferred to an endovascular A treatment team travels to the initial treatment hospital to work with the physician in charge of that hospital for reopening treatment. We have performed more than 160 on-site clot retrieval procedures and have achieved reopening (TICI 2B or higher) in more than 80% of cases.
② Treatment of Chronic Stage Cerebral Infarction
In principle, the brain that has suffered an infarction will not regenerate. Therefore, it is not possible to cure the brain infarction itself. Treatment of chronic stage brain infarction is aimed at preventing recurrence. The main treatments include carotid endarterectomy (CEA) and carotid artery stenting (CAS) for internal carotid artery stenosis, and external carotid artery-internal carotid artery anastomosis (EC-IC) for chronically reduced cerebral blood flow. (bypass) is performed.
③ Moyamoya Disease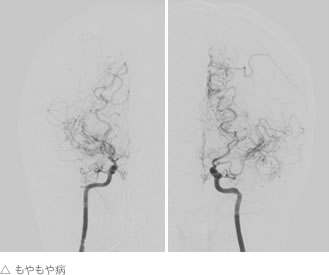
Moyamoya disease is a disease in which the cerebral blood vessels gradually become thinner or clogged.
It is also known as Willis arterial line-blocking disease.
The name “moyamoya disease” comes from the fact that the arteries, which are originally thin, become thicker in order to compensate for the lack of blood flow, and when cerebral angiography is performed, it resembles the sight of cigarette smoke billowing out of a moyamoya. It is said to be more common in East Asian peoples, including the Japanese.
The most common cause of the disease in childhood is cerebral ischemic attack or cerebral infarction due to lack of blood flow, and in adults, it can also be caused by cerebral hemorrhage. The treatment is bypass surgery.
The main method of treatment is to connect blood vessels in the skin to blood vessels on the surface of the brain, but in some cases, the dura mater or some muscles surrounding the brain may be placed on the surface of the brain to wait for smaller blood vessel connections to gradually form.
④ Cerebral Arteriovenous Malformation
A cerebral arteriovenous malformation (AVM) is a condition in which the arteries and veins of the brain are directly connected to each other without capillaries. It can be diagnosed by bleeding or seizures, or it can be detected by chance, such as on an MRI scan.
The rebleeding rate of a bleeding AVM is 5-6% and is treated.
There are two treatment options: 1) surgical resection and 2) radiation therapy (gamma knife, cyber knife, etc.).
Other options include endovascular surgery, but it is difficult to completely cure AVM with endovascular surgery alone and is often performed as a pre-treatment before surgical resection or radiation therapy. The advantage of surgical resection is that once the AVM is completely removed, the risk of bleeding is reduced to zero from that point on.
However, because the AVM itself is located in the brain, it is impossible to remove it without damaging the surrounding brain at all. This increases the risk of postoperative complications if the AVM is in contact with an important part of the brain, and depending on the location, surgery may not be possible. On the other hand, stereotactic radiotherapy, such as the Gamma Knife, has a high probability of eliminating AVMs if the lesion is less than 3 cm in size. However, it takes about 3 years for the AVM to disappear after treatment, and the risk of bleeding does not decrease significantly during this time.
⑤ Dural Arteriovenous Fistula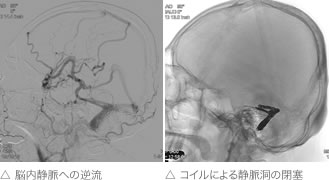
The disease is caused by a direct connection between an artery and a vein on the dura that covers the brain. If only a small amount of blood flows directly into a vein, it will simply return to the heart and is not a big problem.
However, as the amount of blood flowing into the veins increases, the blood can flow back through the veins. When this occurs in the cavernous sinus, a venous sinus behind the eye, the blood flows back through the cancerous veins, causing protrusion and redness of the eye. In more advanced cases, the disease can lead to visual impairment.
If it occurs in the transverse or sigmoid sinus, a venous sinus behind the ear, the patient initially hears ringing in the ears that coincides with the beating of the heart. As blood flow increases, a backflow of veins occurs. When blood flows backwards through the veins that should be returning to the heart from the brain, venous perfusion problems in the brain occur, which can lead to cerebral infarction or brain hemorrhage.
In severe cases, this can lead to stroke or brain hemorrhage. Endovascular therapy is used to block the connection between arteries and veins, but depending on the severity of the disease, it may also be treated with radiation therapy, as described in the AVM section, or surgery.